Current Situation of Care Work in South Korea: 2018 Family Survey
The Care Work and the Economy project’s 2018 fieldwork in South Korea helped us learn a great deal about how childcare and eldercare is provisioned, both in the paid and unpaid care sectors, in Korea.
The fieldwork consisted of both quantitative and qualitative surveys, including two sets of questionnaires for paid care workers and unpaid care providers. The qualitative component consists of two sets of in-depth interview questionnaires for care providers and recipients.
What We Learned about Family Caregiving in Korea
Although many families use at least one external care service to assist with childcare, 22% of respondents reported that their childcare was done only by family members (Kang et al.). Mothers spent six to seven hours more than fathers taking care of children on average.
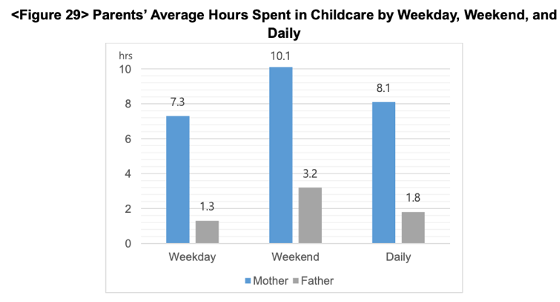
(Kang et al.)
In contrast, 67% of respondents reported that their eldercare was done by family members; the rest reported using external care – usually the national LTC program. The primary caregivers were daughters-in-law (37% of the time), daughters (35%), spouses (15.6%), and sons (11%) (Kang et al.). Figure 12 shows how rather than the elder’s biological children, daughters-in-law provided the most care in terms of time, excepting the elder’s spouse.
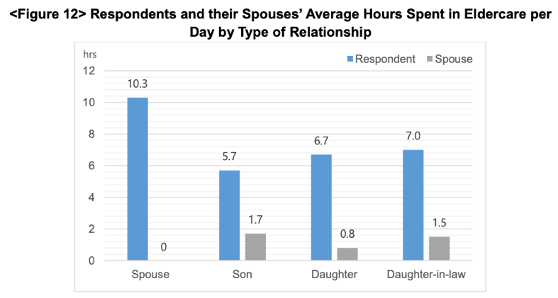
(Kang et al.)
The cost of eldercare is shouldered solely by the primary caregiver in many cases (Kang et al., 2021)
Only 20% of family eldercare providers reported receiving regular financial support from other family members, less than 30% reported receiving help on an irregular basis, and only 8% of those over 65 years old were currently receiving LTC insurance program benefits.
Unpaid care provisioning impacts women’s employment.
The surveys showed that “families in which mothers were the sole caregiver for the child had the highest proportion of unemployed mothers, whereas families that received help with childcare from grandparents or paid care service had the highest proportion of employed mothers. With respect to both types of care arrangements, it was mostly daughters and daughters-in-law serving as primary caregiver, almost 70% of whom were unemployed.” (Kang et al.).
When asked about their preferred hours spent caring, eldercare workers reported a considerably lower number of hours on average than the actual hours they spent caring (see Table 2).
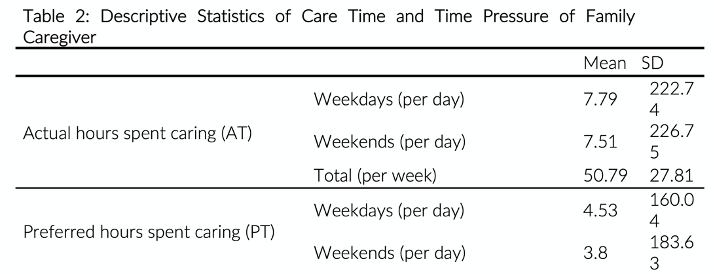
(Cha and Moon,2020)
Studies in the CWE-GAM Project stress concerns about the “quality of the caregiver’s life and the care they provide as well as the quality of life of the care recipient. Especially given that women are typically taking on the role of caregiver, this issue cannot be detached from concerns regarding women’s labor, women’s quality of life, and gender equality in Korea.”
Current Situation in Korea – Government Implications:
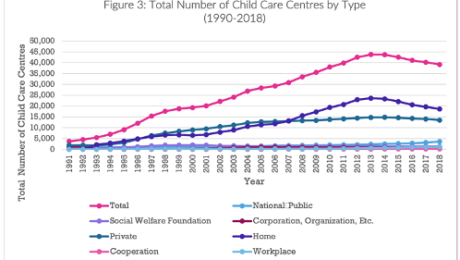
Korea currently “ranks amongst the top 10 OECD countries in terms of public investment in childcare and education” and implemented a mandatory universal LTCI program in 2008 (Peng et al 2021). Figure 2 and 3 show the evolution of child care and care work over time.
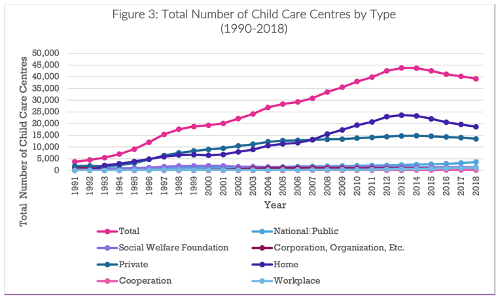
(Peng et al. 2021)
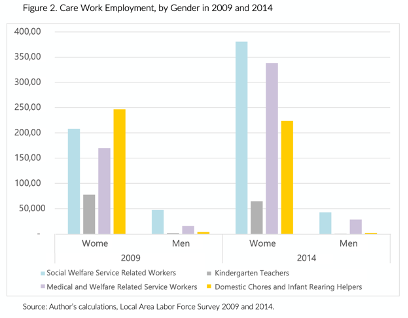
(Suh 2020)
Studies report that despite the social care expansion, “childcare and long-term care sectors are heavily dominated by women, and these care workers are largely poorly paid, over-worked, and precariously employed. Care work is also accorded low social and occupational status, and many care workers experience significant social and emotional stress” (Peng et al. 2021; Suh 2020).
Suh (2020) finds that “public investment in quality care services tends to improve the working conditions of care workers (thereby benefiting care recipients), and unregulated private provision tends to worsen them.”
This suggests that “the government and public sector should drive the effort to meet the multi-faceted challenges posed by the growing demand for care work” (Suh 2020).
“The Korean government […] continues to see care work as an extension of women’s unpaid care work and social care expenditure as something that need to be tightly controlled. A better understanding on the part of policymakers about the importance of care and the role of care work and the care economy in generating employment and positive economic growth and supporting a healthy productive economy is therefore necessary.” (Peng et al.)
This blog was contributed by Aina Krupinski Puig, Research Assistant for the Care Work and the Economy project.
References:
Cha, Seung-Eun, and Hyuna Moon. (2020). “A Glimpse of the Context of Family
Caregivers: Actual Time vs. Preferred Time for Elderly Care.” Care Work and the Economy (CWE-GAM), Program on Gender Analysis in Economics (PGAE), American University. https://doi.org/10.17606/dyfz-jp32.
Kang, Eunhye, Ki-Soo Eun, Jiweon Jun, Seung-Eun Cha, and Hyuna Moon. (2021). “Care
Arrangement and Activities in South Korea: An Analysis of the 2018 Care Work Family Survey on Childcare and Eldercare.” Care Work and the Economy (CWE-GAM), Program on Gender Analysis in Economics (PGAE), American University. https://doi.org/10.17606/8ZYD-AA52.
Peng, Ito, Seung-Eun Cha, and Hyuna Moon. (2021). “An Overview of Care Policies and the
Status of Care Workers in South Korea.” Care Work and the Economy (CWE-GAM), Program on Gender Analysis in Economics (PGAE), American University. https://doi.org/10.17606/EHN0-R646.
Suh, Joo Yeoun. (2020). “Estimating the Paid Care Sector in South Korea.” Care Work and the
Economy (CWE-GAM), Program on Gender Analysis in Economics (PGAE), American University. https://doi.org/10.17606/bpdf-v686.
- Published in Child Care, Elder Care, Paid Care Services, Policy, South Korea, Unpaid Care Work
What is the Care Economy and Why Should We Care?
In our project, we aim to promote and advocate for gender and socioeconomic equalities. We do this by working to reduce gender gaps in economic outcomes and by showing and properly valuing social and economic contributions of caregivers; and integrating care into macroeconomic policy making toolkits.
In this era of demographic shifts, economic change and chronic underinvestment in care provisioning, innovative policy solutions are desperately needed, now more than ever. Sustainable and inclusive development requires gender-sensitive policy tools that integrate new understandings of care work and its connections with labor market supply and economic and welfare outcomes.
The Care Work and the Economy Project, currently based at the Economics Department of American University and co-led by Maria S. Floro and Elizabeth King, includes more than 30 scholars around the globe, working closely together to provide policy makers, scholars, researchers and advocacy groups with gender-aware data, empirical evidence and analytical tools needed to promote creative macroeconomic and social policy solutions. In the next phase of the project, Care Economies in Context, we will be scaling up our project to include 8 different countries, in 4 global regions. I will be leading this next phase of the project, which will be based at the University of Toronto.
I define Care work is defined broadly as work and relationships that are necessary for the health, welfare, maintenance and protection of all people – young and old, able bodied, disabled, and frail. This definition may seem broad – but care– at its core is a very basic human need and a necessity. Whether we know it or now, we all participate in providing care work – paid or unpaid, and in receiving care every day.
By care economy, I am referring to the sector of economy that is responsible for the provision of care and services that contribute to the nurturing and reproduction of current and future populations. More specifically, it involves child care, elder care, education, healthcare, and personal social and domestic services that are provided in both paid and unpaid forms and within formal and informal sectors.
Care work is important because it is important work that sustains life. It is also important now in particular because it is one of the fastest expanding economic sectors and a major driver of employment growth and economic development around the world. For example, across the OCED, the service sector economy now accounts for over 70 percent of total employment and GDP. In lower- and middle-income countries, it is estimated to comprise nearly 60 percent of GDP. Within the service sector economy, care services is one of the fastest growing subsectors.
The International Labour Organization (ILO) estimates that the global employment in care jobs is expected to grow from 206 million to 358 million by 2030 simply based on sociodemographic changes. The figure will be even more dramatic to 475 million if governments invest resources to meet the UN sustainable development goal targets on education, health, long-term care and gender equality.
In Canada, the service sector already makes up for 75 percent of employment and 78 percent of GDP. Within this sector, healthcare, social assistance and education services are key drivers of economic and employment growth. In the U.S., healthcare is already the largest employer, larger than steel and auto industries put together. In short, our current and future economy is and will be increasing dominated by care services and care work.
However, at the same time, much of the care work continues to be performed for no pay, by families and friends, at home and in communities. This unpaid care work is not including in in our national GDP because GDP only takes into account work that is done for pay in the formal market. Therefore, if we only look at the GDP as a measure of the economy and economy growth, we miss a huge segment of the economy and economic activities. As the pandemic has shown, without both paid or unpaid care work, our economy will not be able to function effectively, nor would it be able to sustain itself.
What we are trying to do in our project is to make the care economy clearer and more visible by measuring and mapping out the size and shape of the economy, and to develop macroeconomic models that would help policymakers and civil society actors to develop better policies and better strategies to ensure more sustainable and equality inducing economic growth.
Listen to the full talk “The Care Work and the Economy Project” to learn about what the care economy is and why we should know more about it, particularly now.
The blog was authored by Ito Peng, contributing researcher for the Understanding and Measuring Care research cluster
- Published in Canada, Child Care, Economic Modeling, Elder Care, Expert Dialogues & Forums, Feminist Economics, OECD
LTC Sector Faces a Number of Challenges, Today and Going Forward: An OECD Report
OECD Health Policy Studies has released a 2020 report “Who Cares? Attracting and Retaining Care Workers for the Elderly.” This report addresses a number of important issues while acknowledging the tremendous impact that COVID 19 has had on elderly people and their caretakers. Across OECD countries, more than one out of every six individuals is above the age of 65, and of those roughly 60% live with multiple chronic conditions, making them even more susceptible to the potentially deadly impacts of the virus. Furthermore, many elderly individuals struggle with sufficient access to social support and lack the ability to properly deal with the mental strain of living in a world being affected by a global pandemic.
Beyond these strains, there is a crisis in workforce shortcomings of the Long Term Care (LTC) Sector, which becomes even more problematic in light of the fact that an estimated 50% of COVID 19 related deaths are occurring in LTC facilities. This OECD report begins by addressing many of these shortfalls within the LTC sector, and policies that have the potential to address them.
Within three-quarters of OECD countries, the aging population has outpaced the workforce within the sector since 2011. This is the case even in the countries that have a higher workforce supply than the OECD average such as Japan and the U.S. Within the sector, women make up 90% of the LTC workforce. Attracting a younger workforce has been particularly difficult, and on top of that maintaining workers over the age of 50 is also a challenge. This is even more concerning given that the median age of LTC workers is currently 45.
Many OECD nations have made moves toward relocating their elderly out of facilities and back into the community. This is provoked by the desire to match the preferences of their elderly populations with home-based care, in addition to containing LTC spending. However, a lack of home-based workers has made this challenging, and LTC institution-based workers remain representative of the sector’s workforce across the OECD. This is in large part due to the fact that these institutions cater to the most disabled, which requires a larger workforce. Furthermore, many community-based solutions are not yet equipped to take in these types of complex cases.
The aging of the postwar “baby boom” generation is a factor that will contribute to the increased need for LTC workforce. This also contributes to the predicted increase in labor shortages in the sector to meet the needs of this population going forward. Further, unpaid informal care workers, like that of family members that would care for this aging population, have seen an increase in their own professional workload burdens. When the workload of professional life and caretaking becomes too great, LTC facilities are a means in which to relieve some of that strain. Additionally, as birth rates decline, families become smaller and more women are pursuing professional endeavors, the availability of informal caregivers for the aging population decreases looking into the future. This contributes to another foreseen LTC workforce shortage in the future.

These shortages call for an increase in recruitment within the LTC sector. As the sector workforce ages, attracting younger workers has proven difficult as they, mostly women, are drawn to sectors that have a more appealing image such as a child or hospital care. Additionally, LTC jobs are still widely considered to be feminine positions, and the sentiment on this subject matter has been slow to change.
Foreign-born workers play a significant role in recruiting and retaining LTC workforce. They are highly over representative within LTC across the OECD when compared to other care sectors, and many of them are young, Often, they tend to come into the sector with high levels of skill sets, even overqualified. Micro-econometric analysis has shown that in the U.S. and the UK, these foreign-born workers have higher retention rates than others within the sector.
In terms of recruitment, drumming up interest in the available positions is also problematic. In some cases, many vacancies receive no applications at all. On top of this, recruiters often have a difficult time identifying qualified candidates out of those that do apply.
In order to address this, many countries have focused on four main policies:
– Target recruitment to the traditional pool
– Improve the Image of the sector
-Recruit outside the traditional pool
-Increase the recruitment of for foreign-born workers
Overall, better policies are needed in order to improve recruitment within the LTC sector, and thus far few OECD nations have implemented policies in order to do so. By addressing these issues addressed within the first section of this report, there is potential for effective improvement.
- Published in elderly care, Long Term Care Sector, Policy
Invisible Frontliners: Migrant Care Workers in the Time of COVID-19
The Covid-19 pandemic has exposed fault lines in national healthcare and social protection systems that have made many countries – developed as well as developing – unable to quickly and efficiently deal with this new health crisis and its disastrous consequences on jobs and incomes. One segment of the population in Europe, North America and Asia’s wealthy countries is falling deep into these crevasses, and, sadly, is missing from national debates and policy agendas on the Covid-19 crisis. This group comprises the migrant care workers, especially those who provide care services to elderly, frail, and dependent persons in caregiving institutions and private homes.
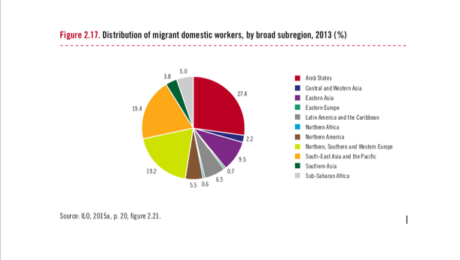
Overwhelmingly consisting of women, these migrant workers (along with minority ethnic groups) are the backbone of the childcare, elderly care and long-term care sectors. They include “nannies”, “home carers”, “social care workers”, “collaboratrice familiar”, nurses and nursing aides, among others. According to the European Commission, workers engaged in “personal and household services” are mostly women, working mainly part-time and often of migrant background. ILO estimates that globally there are 11.5 million international migrant domestic workers, and nearly 80 percent of them are employed in OECD countries. According to data on OECD countries, in 2012–13 28 percent of home-based caregivers were foreign-born.
Increasingly restrictive immigration controls in high-income countries in the past two decades have channelled a disproportionate share of immigrants into jobs in informal long-term and home-based care where wages are low, work hours are long and unpredictable, protection from abuse may be missing, and workload is heavy.[1] These are jobs that can easily be concealed from government surveillance. In the US, UK and Canada, for example, most foreign-born care workers enter the country through non-employment routes, such as family unification, refugee protection and asylum programs, and are on student, tourist and working holiday visas. An unknown number of them work clandestinely.
These migrant care workers are particularly vulnerable in the current Covid-19 pandemic for several reasons. First, eldercare homes across Europe and North America have emerged as hotspots of COVID-19 cases and account for a disproportionate share of deaths related to COVID-19. Data collated by the International Long-term Care Policy Network (hosted by the London School of Economics) across five European countries suggest that between 42 and 57 percent of deaths related to COVID-19 have so far occurred in nursing homes.
Secondly, the disproportionate and increasing share of COVID-19 deaths in eldercare homes is not simply due to the residents’ higher vulnerability due to their age and health conditions. It is also because many caregivers in these homes lack access to PPEs and are often overworked in often understaffed facilities. Being poorly paid, some of them also work in multiple facilities just to make ends meet. Poor working conditions of migrant workers in long-term and eldercare homes have been well documented by several studies – conditions regarding their work hours, allocation of responsibilities for diverse tasks and more difficult patients, low pay rates, and no overtime compensation.
Thirdly, the hundreds of thousands of migrant domestic workers who work in private homes are in the frontlines of keeping homes safe and clean. They face multiple risks as a result of the pandemic – health risks, more demands on their time, and income loss. According to the International Domestic Workers Federation, domestic workers worldwide have reported many concerns since the global pandemic began. With entire families staying home all day due to quarantine measures, domestic workers face heavier demands of cooking, cleaning, and caregiving without the benefit of additional pay for longer hours—and because of mobility restrictions, many cannot leave the homes where they work.
Finally, many care workers who have irregular migrant and/or employment status under informal arrangements have no access to unemployment and health insurance benefits, relief packages or financial aid related to COVID-19. This has been recently documented by the National Domestic Workers Alliance and the Pennsylvania Domestic Workers Alliance (networks representing nannies, caregivers and domestic workers in the US), the European Trade Union, and the Kanlungan Filipino Consortium in the UK. Those who fall ill prefer not to go to hospitals until it is too late for fear of being reported to migration authorities and because they do not have health insurance. These care frontliners are largely invisible and likely to suffer in silence
Contributed by Amy King-Dejardin, Former senior staff of ILO (Geneva) and author of the 2018 ILO report, “The Social Construction of Migrant Care Work.”
[1] King-Dejardin, A., 2019, The social construction of migrant care work, Geneva: ILO https://www.ilo.org/global/topics/labour-migration/publications/WCMS_674622/lang–en/index.htm
*Learn more about the ILO Bureau of Gender Equality here
- Published in COVID 19, Migrant Care Workers